CLICK TO SHOP OUR BLACK FRIDAY SALE!
*Excludes BioNude and subscriptions
If your bladder feels like it’s staging a protest - pain, urgency, or that maddening feeling of needing to go even when tests are “clean” - you’re in the right place. This post unpacks why bladder and vulvovaginal pain often overlap (hint: menopause-driven tissue changes and shifts in the vaginal microbiome are major players), how to tell these problems apart from a UTI or an STI, what commonly lights the fuse (from scented products to certain foods and pelvic-floor tension), and practical, evidence-informed things that can actually help - everything from simple product swaps and diet tweaks to pelvic-floor therapy and targeted local estriol for menopausal folks. Read on for clear, no-nonsense explanations and actionable steps you can try tonight.
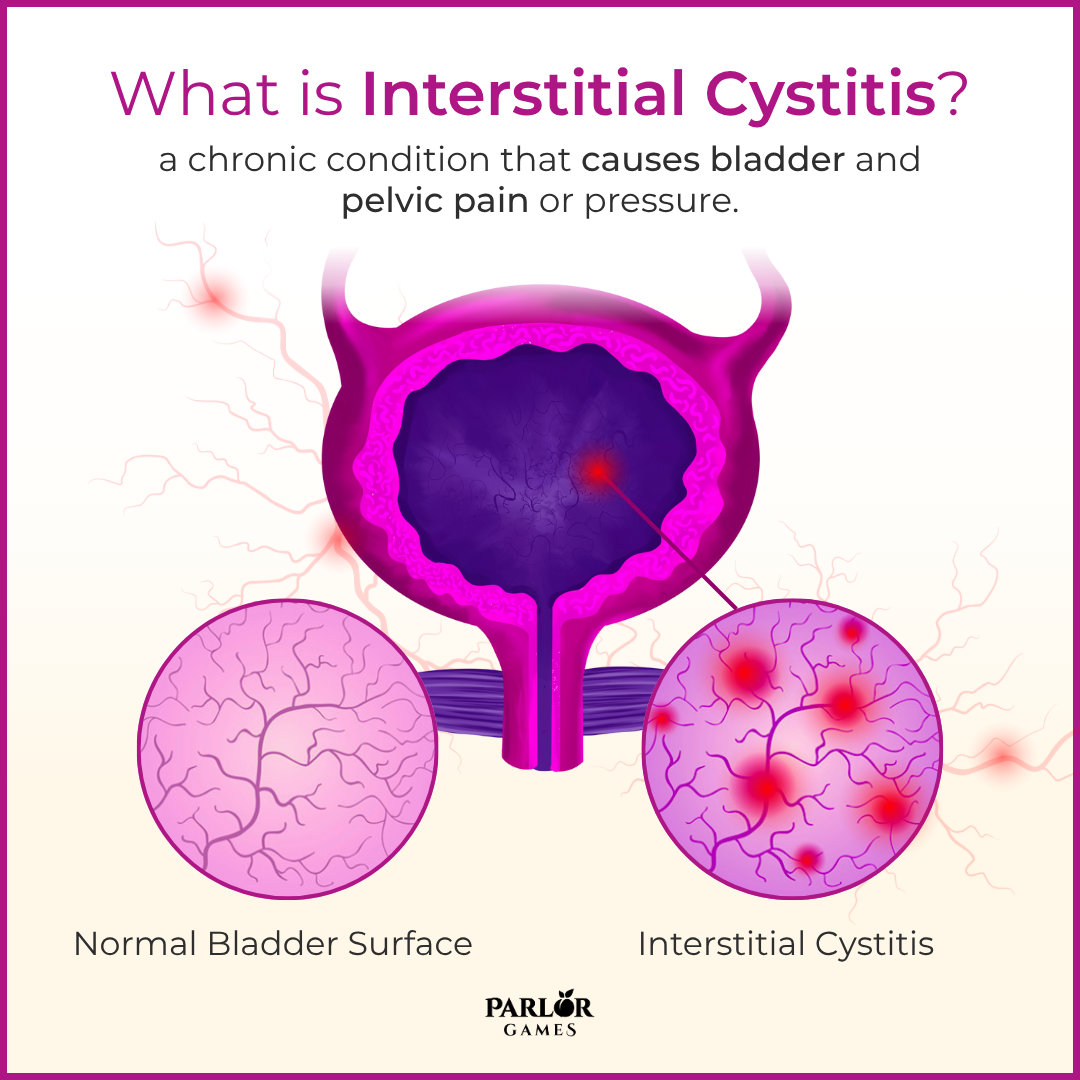
Interstitial Cystitis (IC), is a chronic condition causing bladder pressure, bladder pain, and sometimes pelvic pain, and - it is something we get asked about a lot. Namely, can Silky Peach help with IC?
Our response? YES! IC is a disease of undetermined cause; however, inflammation is thought to be a key player.
This study found that, “there was a significant positive effect of local estrogen therapy on urinary and sexual function following 12 weeks, as well as an improvement of vaginal health. The results of this open study indicate that 12 weeks of local estriol cream at vaginal and vestibular-level may ameliorate urinary/bladder pain symptoms, and may improve sexual function. The association between vulvar pain and bladder pain could, therefore, be related to a vaginal environment carrying signs of hypoestrogenism, (too little estrogen) but further studies are needed to clarify this issue.”
Now, if you don’t have a degree in biochem, here is what that means in people-ese. The cells in the pelvis, around the bladder, the vagina, and the whole perineum have lots of receptors for estrogen. If the body puts receptors there, then estrogen will have a necessary effect on those cells. Estrogen is important for keeping cells healthy, for building their ability to fight bacterial invaders, and have a strong immune function. As estrogen drops at menopause and beyond, we no longer have the supply of estrogen to help those cells to stay healthy. This often results in low grade chronic infections in the vagina, the bladder, and the urethra. The pH level in these areas starts to rise and that increases the chance that bacteria can take hold, which contributes further to the inflammation.
A lot of things can light the fuse on bladder and vulvovaginal pain — sometimes it’s obvious, sometimes it’s sneaky. Common triggers to call out:
Some people with bladder sensitivity find that certain foods and beverages reliably make symptoms worse. Try a short elimination trial (a week or two) to see what affects you — individual patterns matter. Common offenders:
Applied inside the vagina, low-dose estriol helps rebuild the lining and restore glycogen, so the environment becomes more acidic again and protective Lactobacillus are more likely to return. That repair process lowers local inflammation, improves tissue resilience, and can reduce both vaginal and nearby bladder pain for many people — which is exactly why clinicians see benefit in some patients with IC-type symptoms. (Yes, it can sting at first; that’s usually inflammation settling down.)
Using estriol cream - such as Silky Peach - can gradually rebuild the amount of estriol in the whole area. A good analogy is that of a sponge; imagine a dried out sponge that gets a drop of water added every day, eventually it will swell back up. Thus, with levels of estriol increased, the body has a better ability to fight off infection.
The cream may have a stinging sensation to begin with; this is because the skin is likely raw and inflamed and adding anything will sting, no matter what. Over time, the cells will rejuvenate. The acidity will increase again (a good thing) and the ability of the body to overcome infection will be improved. There are other steps you can take to help ensure you have healthy inner skin – read our Top tips for your ladybits.
We will add - if the stinging does not clear up - it’s time for a heart to heart with your doctor about some prescription strength estriol solutions to get you past the worst of it before carrying on with a regular therapeutic treatment...like Silky Peach!

Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
Parlor Games, LLC ● kate@parlor-games.com ● 5304 River Rd N Ste B ● Keizer OR 97303
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
28 Day Challenge Subscription Details

We ship you a 28 day supply of Silky Peach Cream for only $29 (more than 25% off our normal price) when you sign up for Subscribe & Save.
Follow the directions we include in the package and apply Silky Peach cream on your tender bits for 28 days.

Decision Day:
5 days before your subscription rebills, we’ll send you an email reminder with a link. If you decide Silky Peach is nice but not your thing… you can click that link and cancel your subscription without even talking to anyone. No hassle — no questions asked.
If you are like 72% of our Silky Peach customers, you’ll love it and can't imagine life without it. In that case, do nothing, and we’ll welcome you to the Parlor Games family and ship Silky Peach Cream to your door step every month for the same discounted price of $29 — locked in for as long as you remain a subscriber.

Important note about our easy-breezy subscriptions:
We know that some companies make it hard to cancel a subscription — that’s not us. Our mission is to save the world — one vagina at a time! If you decide you don’t need Estriol as an ongoing solution for dryness, incontinence, UTIs and keeping sex fun and comfortable again, we understand. Five days before we ship your next order, you'll receive an email with a link to cancel right there in the message.
No hunting, no searching, we got you. Respect is where it’s at.
FYI – Estriol is beneficial for skin integrity and mucous membranes. It’s great for vaginal atrophy and also amazing for use on the face and neck. Applying a small amount — about 1 pump — can help build the collagen and plump up the cells to reduce wrinkles. Who knew!!
OUR HAPPINESS GUARANTEE
We want you to feel safe and confident trying any of our products. That's why we promise 100% money-back guarantee on the purchase price of the first bottle of any of our products. Balancing hormones DOES take some time, so please try it for 28 days. If after 28 days you are unhappy, or the product just hasn't worked for you, simply contact us and we'll process a refund of your full purchase price upon receipt. Sorry, shipping fees are not refundable.