CLICK TO SHOP OUR BLACK FRIDAY SALE!
*Excludes BioNude and subscriptions
Your vagina’s microbiome is way more interesting (and more easily confused) than you probably think - and not every weird smell, discharge, or itch is bacterial vaginosis (BV). In this blog we’ll walk through the common things that can mimic BV, what modern swabs and lab tests actually tell us (and when testing matters), when hormone checks are useful versus when a short trial of local estrogen makes more sense, the bigger causes that set the scene, and how simple gut-friendly moves like adding fiber can help your vaginal defenses.
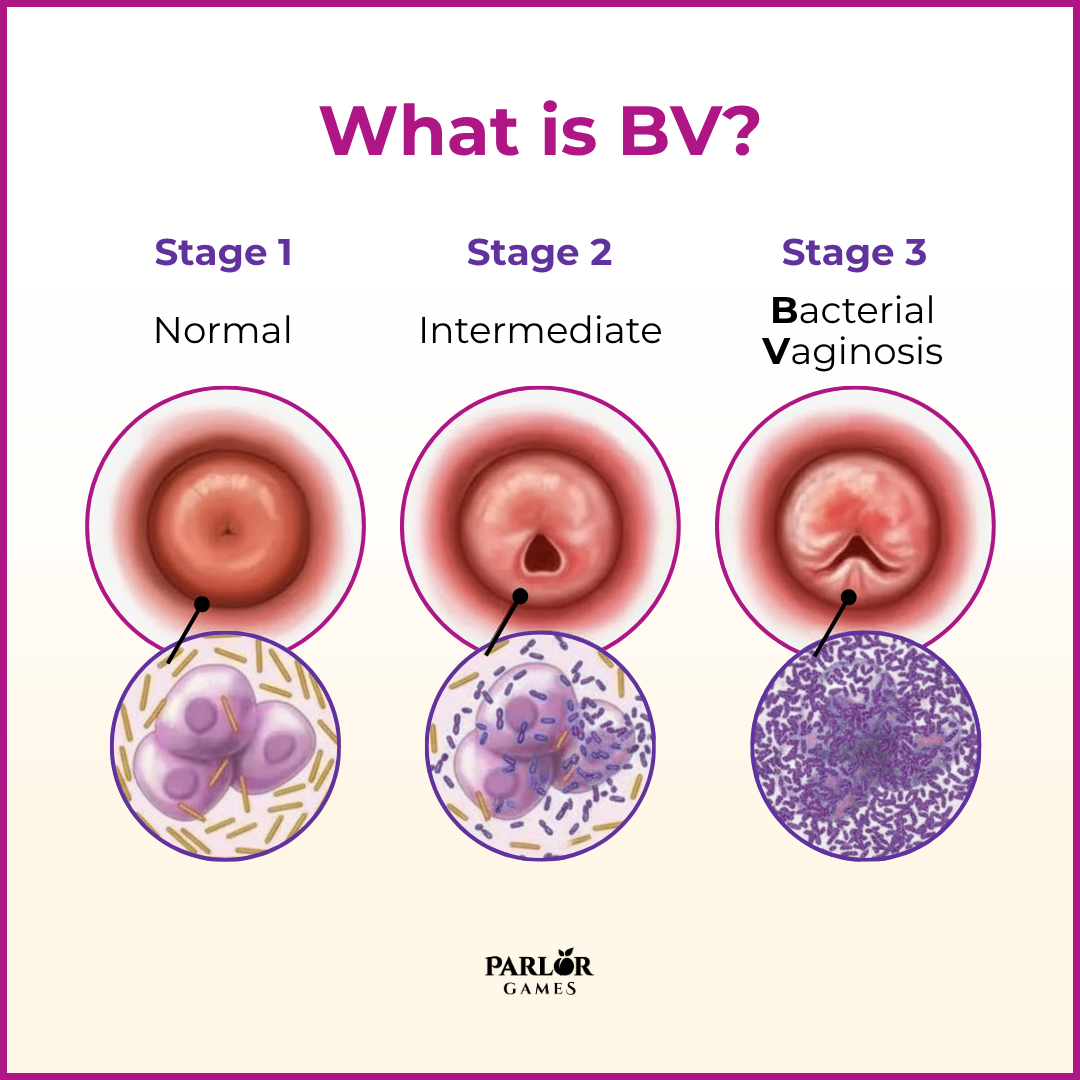
Bacterial vaginitis (BV) isn’t, as many women think, an infection with a specific bacteria or yeast. BV refers to an imbalance in the vagina’s own bacterial communities. When beneficial organisms aren’t as robust, it can lead to an overgrowth of the less-than-desirable bacteria in the vagina (Peptostreptococcus species, Eubacterium species, Mobiluncus species, Gardnerella, and Mycoplasma hominis, Gardnerella vaginalis, to name just a few!).
• A white vaginal discharge that covers the walls of the vagina
• Vaginal discharge with a foul or fishy odor
• Vaginal pain or itching
• Burning while urinating
An imbalance between good/healthy bacteria and bad/unhealthy bacteria is the cause for the inflammation that causes this condition. Several factors can make a female more prone to the development of bad bacteria such as:
• Gut dysbiosis
• High sugar diet, alcohol consumption, or poorly controlled blood sugar
• Exposure to synthetic chemicals/fragrances that upset beneficial bacteria or vaginal pH
• Repeated antibiotic use
• Stress
• Changes in the vaginal pH that can happen with age.
- Recurrent or broad-spectrum antibiotic exposure — knocks back lactobacilli and can set the stage for dysbiosis.
- High simple-sugar diets and poorly controlled blood sugar — emerging data link diet and carbohydrate intake with vaginal microbiota shift.
- Smoking — associated with higher BV risk in observational studies.
- Obesity and chronic inflammation — systemic inflammation may alter local mucosal immunity.
- Hormonal contraceptives & menstrual products — menstrual blood and some product chemistries can temporarily shift pH and microbes.
- Immune suppression and chronic stress — both change local defenses and pain perception.
- Smoking — associated with higher BV risk in observational studies.
- Obesity and chronic inflammation — systemic inflammation may alter local mucosal immunity.
- Hormonal contraceptives & menstrual products — menstrual blood and some product chemistries can temporarily shift pH and microbes.
- Immune suppression and chronic stress — both change local defenses and pain perception.
Recognizing that multiple factors often stack together helps explain why BV recurs in many people and why a single antibiotic course sometimes fails.
Currently BV is treated in isolation - using an antibiotic cream to remove the overgrowth of harmful bacteria. Metronidazole has an 80 percent cure rate within 4 weeks, but the recurrence rate is disproportionately high: 15 to 50 percent of women who treat BV with metronidazole experience a return of symptoms within 3 months! Antibiotics also remove the healthy bacteria important for vaginal health. We want that vaginal flora to flourish in all the right ways, so that your lady garden can maintain the right pH and you can be BV free.
If symptoms are recurrent, severe, or treatment-resistant, clinicians may use one or more of these approaches:
Several different problems can cause discharge, itching, odor or burning — and they’re often mistaken for bacterial vaginosis (BV). Common look-alikes include:
Alternative non-antibiotic options such as probiotic products containing lactobacilli, lactic acid, sucrose gel, and combination products with estriol, are starting to get more attention. This is because they are able to target the problem without annihilating the good bacteria.
Estriol in the Silky Peach Cream is definitely part of the process - along with getting the right bacteria in place and making sure the inner sanctum has the right pH to allow the right bacteria to grow. The key to clearing up BV for good is to get to the root cause. If BV has been a naggingly persistent issue, a naturopathic practitioner or homeopathic practitioner will have some good ideas on ways to discover and heal the root cause.
The gut and vaginal microbial communities talk to one another. Species can travel (or share metabolites), and diet shapes the gut community — which in turn influences the vaginal environment. Practical, evidence-informed points:
Estrogen plays a crucial role in maintaining the vaginal pH balance. It stimulates the production of glycogen in the vaginal lining, which serves as a food source for beneficial bacteria called lactobacilli. These lactobacilli thrive on glycogen and produce lactic acid as a byproduct. Lactic acid helps lower the vaginal pH, creating an acidic environment that inhibits the growth of harmful bacteria and yeast, thus promoting vaginal health.
What success (or troubles) have you had with BV? We always love to hear from you as we try to save the world, one vagina at a time!

Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
Parlor Games, LLC ● kate@parlor-games.com ● 5304 River Rd N Ste B ● Keizer OR 97303
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
28 Day Challenge Subscription Details

We ship you a 28 day supply of Silky Peach Cream for only $29 (more than 25% off our normal price) when you sign up for Subscribe & Save.
Follow the directions we include in the package and apply Silky Peach cream on your tender bits for 28 days.

Decision Day:
5 days before your subscription rebills, we’ll send you an email reminder with a link. If you decide Silky Peach is nice but not your thing… you can click that link and cancel your subscription without even talking to anyone. No hassle — no questions asked.
If you are like 72% of our Silky Peach customers, you’ll love it and can't imagine life without it. In that case, do nothing, and we’ll welcome you to the Parlor Games family and ship Silky Peach Cream to your door step every month for the same discounted price of $29 — locked in for as long as you remain a subscriber.

Important note about our easy-breezy subscriptions:
We know that some companies make it hard to cancel a subscription — that’s not us. Our mission is to save the world — one vagina at a time! If you decide you don’t need Estriol as an ongoing solution for dryness, incontinence, UTIs and keeping sex fun and comfortable again, we understand. Five days before we ship your next order, you'll receive an email with a link to cancel right there in the message.
No hunting, no searching, we got you. Respect is where it’s at.
FYI – Estriol is beneficial for skin integrity and mucous membranes. It’s great for vaginal atrophy and also amazing for use on the face and neck. Applying a small amount — about 1 pump — can help build the collagen and plump up the cells to reduce wrinkles. Who knew!!
OUR HAPPINESS GUARANTEE
We want you to feel safe and confident trying any of our products. That's why we promise 100% money-back guarantee on the purchase price of the first bottle of any of our products. Balancing hormones DOES take some time, so please try it for 28 days. If after 28 days you are unhappy, or the product just hasn't worked for you, simply contact us and we'll process a refund of your full purchase price upon receipt. Sorry, shipping fees are not refundable.