CLICK TO SHOP OUR BLACK FRIDAY SALE!
*Excludes BioNude and subscriptions
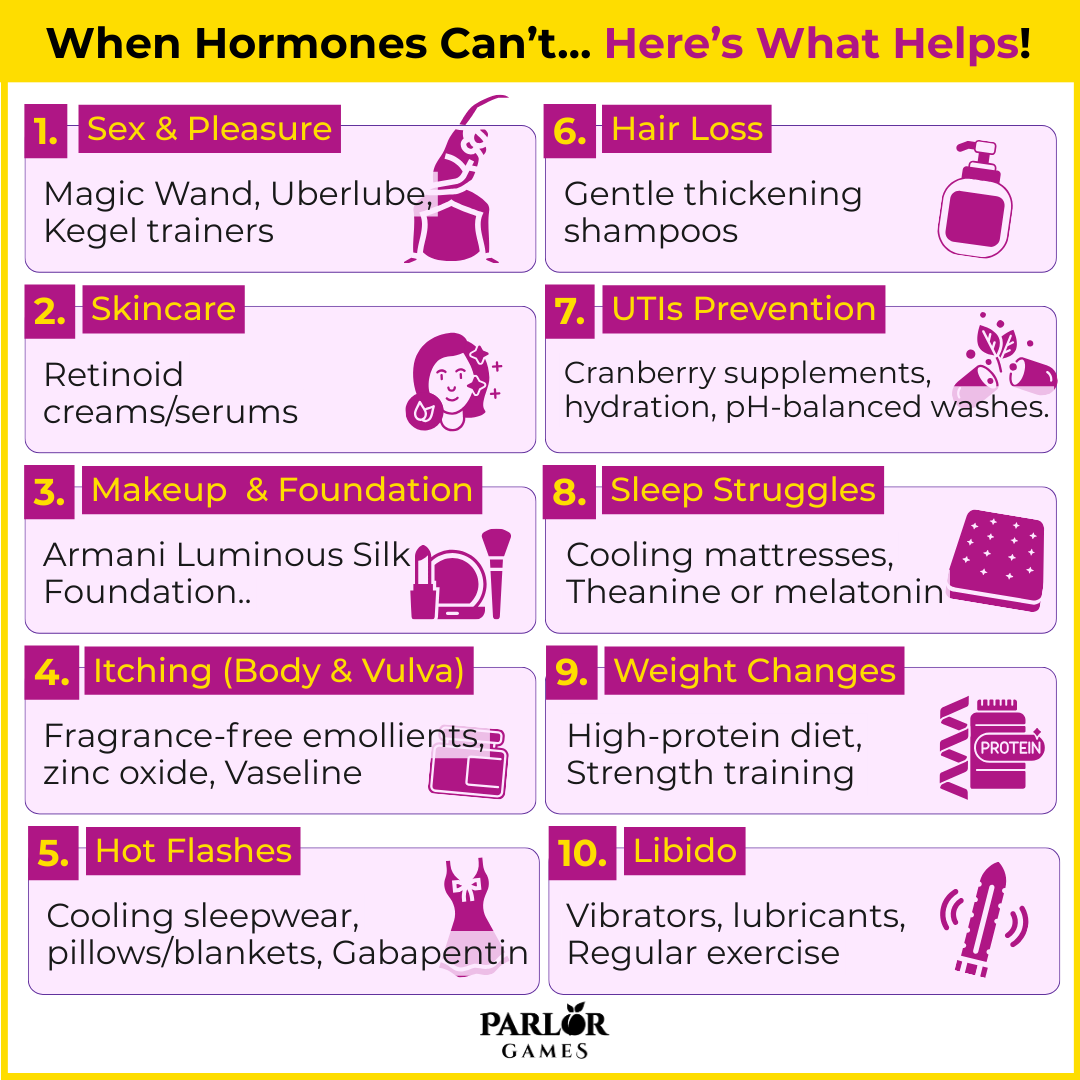
Wondering what to use when it comes to skincare, UTI relief, itching, or any of those other fun, fabulous... and downright weird parts of menopause and aging? We've got you covered - from our ladies inside our private group, to the latest scientific research, here are the products that can help when hormones can't!
Why it happens:
Declining estrogen and testosterone reduce genital blood flow, tissue elasticity, and natural lubrication. Many women report less arousal and more discomfort, which can snowball into reduced desire.
What helps (women & science recommend):
Why:
Vibratory stimulation increases genital blood flow and nerve activation, helping counteract the arousal lag of menopause. Iso-osmolar and silicone lubes minimize mucosal irritation by protecting epithelial cells, while pelvic floor exercises improve circulation, orgasm response, and continence.
Why it happens:
Estrogen supports collagen, elastin, and oil production. After menopause, skin becomes drier, thinner, and itchier. The barrier weakens, leading to irritation and sensitivity.
What helps:
Why:
Ceramides and humectants restore the skin barrier and retain water. Urea helps with desquamation (flaky buildup). Retinoids increase collagen synthesis and improve dermal thickness, which declines with estrogen loss. Sunscreen prevents accelerated photoaging that compounds hormonal skin thinning.
Why it happens:
Drier, thinner skin with more fine lines makes makeup settle into creases. Sebum production drops, so heavy powders and mattes can look mask-like.
What helps:
Why:
These formulas use lightweight emollients and humectants to create a smoother, more radiant finish without clinging to texture. Dewy foundations mimic the lost “natural oils” of younger skin, preventing a dull, flat look.
Why it happens:
Low estrogen means fewer lipids and glycosaminoglycans in skin and mucosa. The vulvar epithelium thins, becoming drier and more sensitive, while body skin gets rough and flaky.
What helps:
Why:
Occlusives (petrolatum, zinc oxide) reduce transepidermal water loss and shield fragile vulvar skin. Cotton fabrics lower friction and dampness that worsen irritation. Urea and lactic acid gently exfoliate while hydrating body skin.
Why it happens:
Estrogen withdrawal destabilizes the hypothalamus, the brain’s thermostat, making it trigger “false heat alarms.” The result: sudden flushing, sweating, and disrupted sleep.
What helps:
Why:
Cooling fabrics improve comfort but don’t stop the physiological trigger. SSRIs/SNRIs regulate serotonin pathways that influence thermoregulation. Gabapentin reduces neuronal excitability linked to hot flashes. Fezolinetant blocks NK3 receptors on KNDy neurons, directly addressing the hot-flash mechanism.
Why it happens:
Post-menopause, estrogen and progesterone decline while androgen activity becomes unopposed, shrinking hair follicles (female pattern hair loss).
What helps:
Why:
Minoxidil prolongs the follicle’s growth phase (anagen), reversing miniaturization. Low-level laser therapy stimulates mitochondria in dermal papilla cells, encouraging regrowth. Cosmetic thickening shampoos give temporary volume by coating hair strands.
Why it happens:
Estrogen decline weakens the vaginal microbiome (less lactobacillus), lowering acidity and allowing uropathogens like E. coli to colonize more easily.
What helps:
Why:
Cranberry PACs reduce bacterial adhesion to bladder cells. Hydration dilutes bacteria and supports flushing. Avoiding harsh soaps helps maintain natural microbiota balance.
Why it happens:
Hot flashes, cortisol dysregulation, and reduced melatonin all contribute to fragmented sleep. Stress and mood changes amplify the cycle.
What helps:
Why:
CBT-I restructures maladaptive sleep behaviors and shows durable benefits in RCTs. Weighted blankets improve parasympathetic tone. Cooling surfaces offset thermoregulatory instability. Magnesium and theanine modulate GABAergic pathways; melatonin helps realign circadian rhythms.
Why it happens:
Declining estrogen shifts fat storage from hips/thighs to the abdomen. Muscle mass drops, metabolism slows, and insulin resistance rises.
What helps:
Why:
Resistance training and protein intake stimulate muscle growth via mTOR, supporting metabolic rate. HIIT enhances insulin sensitivity. Mindful eating reduces cortisol-driven overeating and improves body awareness.
Why it happens:
Hormonal shifts, reduced blood flow, vaginal dryness, body image changes, and fatigue can all dampen sexual desire. Psychological factors, like stress and relationship strain, amplify the challenge.
What helps:
Why:
Libido depends on dopamine, norepinephrine, and vascular response. Vibrators/lubes reduce barriers to arousal. Mindfulness restores cognitive engagement in desire. Exercise improves endorphins, body image, and blood flow. Bupropion, unlike SSRIs, enhances dopaminergic tone and has shown benefits for desire in clinical studies.
NOTE: These are sourced from several places, including our private group (the Sexy Sassy Sisterhood), our team, Facebook, and Reddit. These are anecdotal, although some are supported by science (see References below). If you have serious medical issues, please reach out to your doctor!
References

Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
Parlor Games, LLC ● kate@parlor-games.com ● 5304 River Rd N Ste B ● Keizer OR 97303
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
28 Day Challenge Subscription Details

We ship you a 28 day supply of Silky Peach Cream for only $29 (more than 25% off our normal price) when you sign up for Subscribe & Save.
Follow the directions we include in the package and apply Silky Peach cream on your tender bits for 28 days.

Decision Day:
5 days before your subscription rebills, we’ll send you an email reminder with a link. If you decide Silky Peach is nice but not your thing… you can click that link and cancel your subscription without even talking to anyone. No hassle — no questions asked.
If you are like 72% of our Silky Peach customers, you’ll love it and can't imagine life without it. In that case, do nothing, and we’ll welcome you to the Parlor Games family and ship Silky Peach Cream to your door step every month for the same discounted price of $29 — locked in for as long as you remain a subscriber.

Important note about our easy-breezy subscriptions:
We know that some companies make it hard to cancel a subscription — that’s not us. Our mission is to save the world — one vagina at a time! If you decide you don’t need Estriol as an ongoing solution for dryness, incontinence, UTIs and keeping sex fun and comfortable again, we understand. Five days before we ship your next order, you'll receive an email with a link to cancel right there in the message.
No hunting, no searching, we got you. Respect is where it’s at.
FYI – Estriol is beneficial for skin integrity and mucous membranes. It’s great for vaginal atrophy and also amazing for use on the face and neck. Applying a small amount — about 1 pump — can help build the collagen and plump up the cells to reduce wrinkles. Who knew!!
OUR HAPPINESS GUARANTEE
We want you to feel safe and confident trying any of our products. That's why we promise 100% money-back guarantee on the purchase price of the first bottle of any of our products. Balancing hormones DOES take some time, so please try it for 28 days. If after 28 days you are unhappy, or the product just hasn't worked for you, simply contact us and we'll process a refund of your full purchase price upon receipt. Sorry, shipping fees are not refundable.