LAST DAY TO SAVE 10%* - Coupon BFCM2024
*Excludes BioNude, subscriptions, hormone tests and health coaching
Midlife acne isn’t just real—it’s common, underdiagnosed, and often mismanaged. So, what’s causing these unwelcome eruptions? And more importantly, what can you actually do about it?
Let’s talk about why we break out in perimenopause and menopause, how acne works in the body, and what helps (and hurts) when it comes to clearing things up.
Acne is a chronic inflammatory skin condition that starts in the pilosebaceous unit—the combo of your hair follicle and its attached oil gland (sebaceous gland). When that unit gets clogged with excess oil (sebum), dead skin cells, and sometimes bacteria like Cutibacterium acnes, inflammation sets in.
That inflammation can show up as:
The key driver behind all of this? Hormones. Particularly androgens, which increase oil production in the skin.
Here’s the hormonal plot twist: while estrogen and progesterone levels begin to decline in perimenopause, androgens (like testosterone and DHEA) decline more slowly—or in some cases, remain stable.
This shift creates a hormonal imbalance where androgens become relatively dominant compared to estrogen and progesterone. That androgen dominance stimulates the sebaceous glands, increases sebum production, and thickens the skin’s outer layer (stratum corneum), leading to more clogged pores.
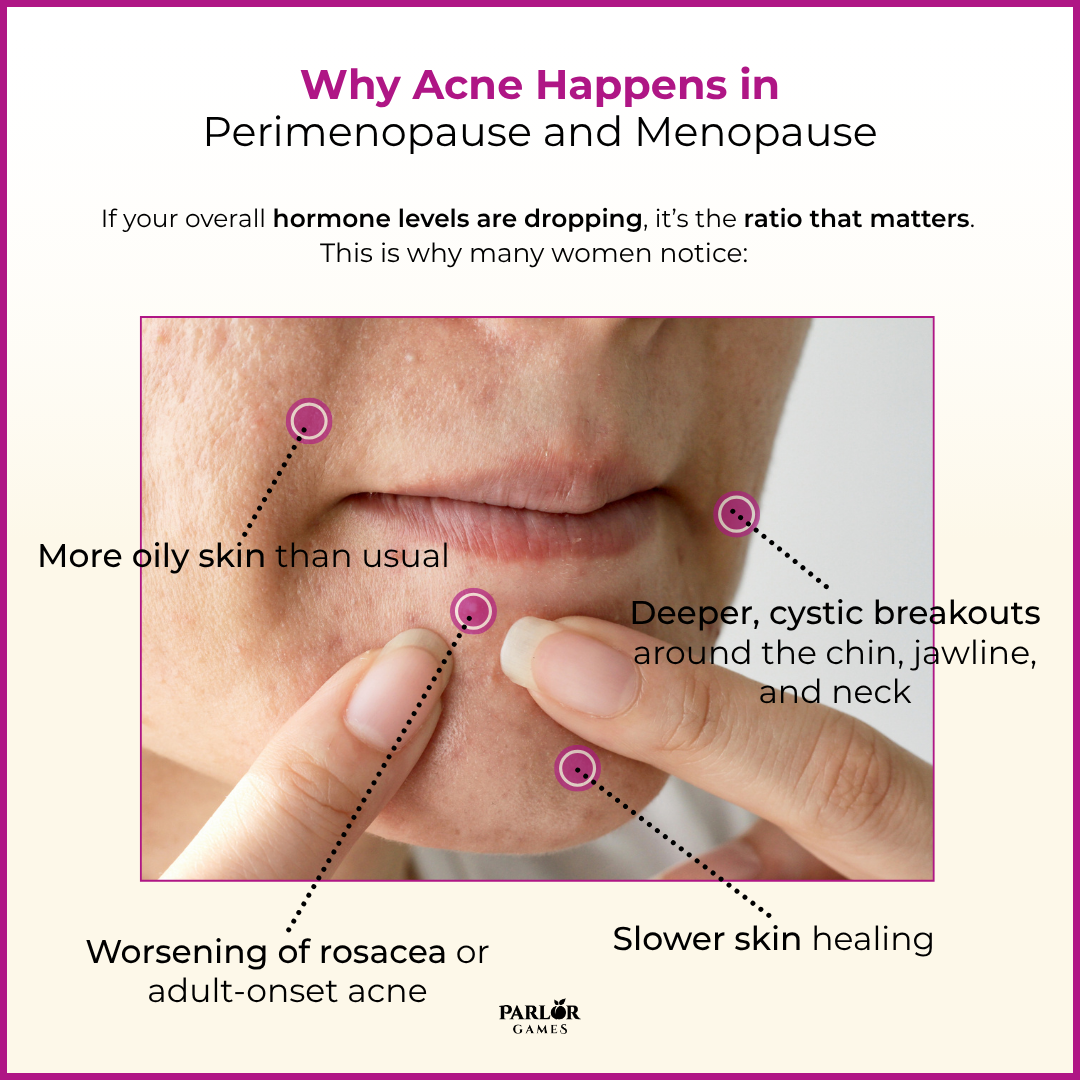
So even if your overall hormone levels are dropping, it’s the ratio that matters. This is why many women notice:
This hormonal landscape often goes hand-in-hand with increased insulin resistance and cortisol dysregulation—two more players that can worsen skin health.
Let’s unpack how key hormones affect your skin:
As estrogen declines, the skin loses some of its anti-inflammatory protection—and oil control.
The bottom line: when estrogen and progesterone are low, and androgens and cortisol are relatively high, your skin takes the hit.
Some of the most well-intentioned fixes can backfire. Here’s what often worsens midlife acne:
Here’s the evidence-based skin support strategy, both inside and out:
Avoid benzoyl peroxide if your skin is mature or dry—it can be too harsh and barrier-damaging.
If you’ve tried everything and acne persists, it’s worth running:
This helps identify if acne is primarily androgen-driven, cortisol-driven, or a mix.
Adult acne comes with a cruel kind of whiplash. You're managing careers, kids, aging parents, maybe hot flashes—and you're breaking out like a teen.
For many women, acne in midlife brings a sense of shame, frustration, and isolation. Studies show that adult women with acne report significant body image dissatisfaction, social withdrawal, and even depressive symptoms. One survey found that more than 60% of women over 40 with acne said it impacted their self-esteem and social interactions (Tanghetti et al., 2014).
And because adult female acne isn’t talked about much—especially in perimenopause—it’s often dismissed as a cosmetic problem rather than a legitimate hormonal red flag.
Perimenopausal acne is your body trying to tell you something: that your hormones are shifting, your skin needs support, and your stress response may be tapped out.
Whether it’s a few pesky spots or painful cysts, know that this is not about hygiene or bad luck—it’s biology.
📦 Rebalance from the inside out... Try Vibrant Third Progesterone and Silky Peach Estriol for a topical, bioidentical hormone approach that supports skin health, hormone balance, and a calmer nervous system.
Because midlife skin deserves love, not shame.

Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Lorem ipsum dolor sit amet, consectetur adipiscing elit.
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
Parlor Games, LLC ● kate@parlor-games.com ● 5304 River Rd N Ste B ● Keizer OR 97303
Disclaimer: The information provided above is intended for educational and informational purposes only. Statements made have not been evaluated by the FDA nor are they intended to treat or diagnose. Any health concerns should be discussed and evaluated by your primary health care provider.
28 Day Challenge Subscription Details

We ship you a 28 day supply of Silky Peach Cream for only $29 (more than 25% off our normal price) when you sign up for Subscribe & Save.
Follow the directions we include in the package and apply Silky Peach cream on your tender bits for 28 days.

Decision Day:
5 days before your subscription rebills, we’ll send you an email reminder with a link. If you decide Silky Peach is nice but not your thing… you can click that link and cancel your subscription without even talking to anyone. No hassle — no questions asked.
If you are like 72% of our Silky Peach customers, you’ll love it and can't imagine life without it. In that case, do nothing, and we’ll welcome you to the Parlor Games family and ship Silky Peach Cream to your door step every month for the same discounted price of $29 — locked in for as long as you remain a subscriber.

Important note about our easy-breezy subscriptions:
We know that some companies make it hard to cancel a subscription — that’s not us. Our mission is to save the world — one vagina at a time! If you decide you don’t need Estriol as an ongoing solution for dryness, incontinence, UTIs and keeping sex fun and comfortable again, we understand. Five days before we ship your next order, you'll receive an email with a link to cancel right there in the message.
No hunting, no searching, we got you. Respect is where it’s at.
FYI – Estriol is beneficial for skin integrity and mucous membranes. It’s great for vaginal atrophy and also amazing for use on the face and neck. Applying a small amount — about 1 pump — can help build the collagen and plump up the cells to reduce wrinkles. Who knew!!
OUR HAPPINESS GUARANTEE
We want you to feel safe and confident trying any of our products. That's why we promise 100% money-back guarantee on the purchase price of the first bottle of any of our products. Balancing hormones DOES take some time, so please try it for 28 days. If after 28 days you are unhappy, or the product just hasn't worked for you, simply contact us and we'll process a refund of your full purchase price upon receipt. Sorry, shipping fees are not refundable.